Introduction
Feline diabetes mellitus is a metabolic disorder characterized by inadequate insulin production or insulin resistance, leading to persistent high blood glucose levels. Early recognition and proper management can help cats lead healthier, less symptom-burdened lives.
1. Recognizing Symptoms
Polydipsia (Increased Thirst): Diabetic cats often drink disproportionately more water to flush excess glucose through urine.
Polyuria (Frequent Urination): You may notice damp spots in the litter box or around the house.
Polyphagia (Increased Appetite): Despite eating more, diabetic cats can still lose weight because they cannot utilize glucose properly.
Weight Loss & Muscle Wasting: Catabolic processes accelerate when glucose remains unused, leading to rapid weight loss.
Lethargy & Weakness: High blood glucose can cause fatigue, decreased grooming, and reduced playfulness.
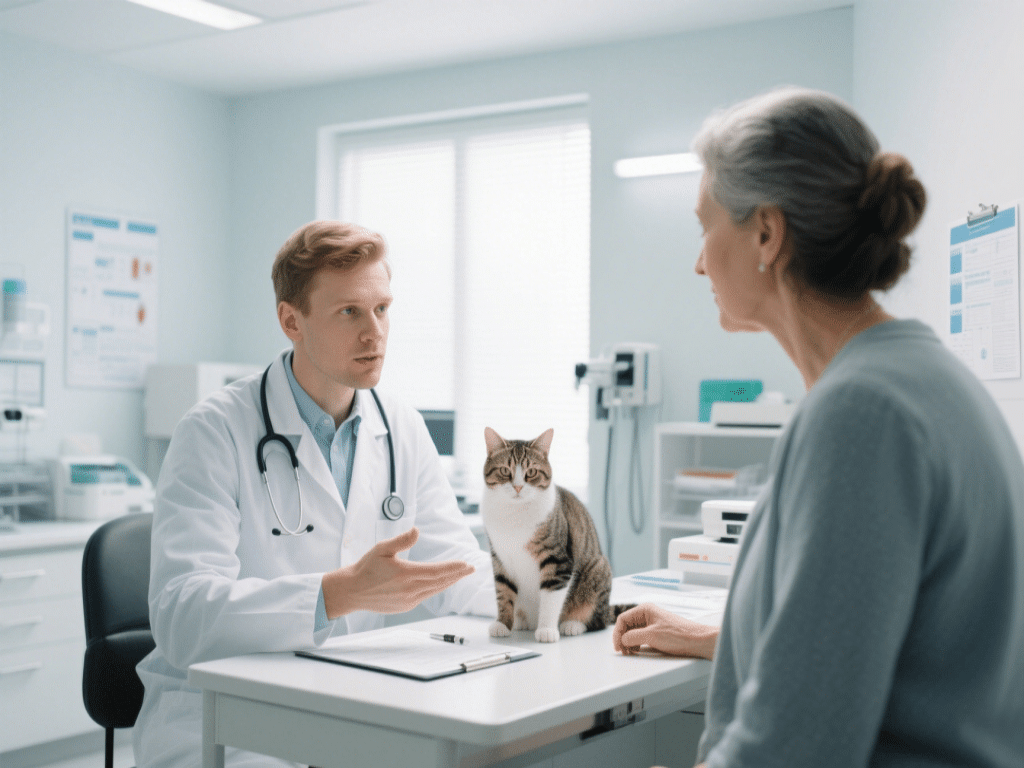
2. Diagnosis
Blood Glucose Testing: A central diagnostic tool. Elevated fasting blood glucose (>200 mg/dL) raises suspicion.
Fructosamine Levels: Reflect average glucose control over 2–3 weeks, offering insight into long-term glycemic status.
Urinalysis: The presence of glucose and possibly ketones in urine confirms hyperglycemia.
3. Dietary Management
High-Protein, Low-Carbohydrate Diets: Cats evolved as obligate carnivores; restricting carbohydrates and emphasizing protein stabilizes blood sugar.
Portion Control & Meal Scheduling: Offer multiple small meals at consistent times—ideally around insulin injections—to avoid glucose spikes.
Prescription Diets: Veterinary-formulated diabetic diets (dry or canned) ensure balanced ratios of protein, fat, and minimal carbs.
4. Insulin Therapy
Insulin Types: Long-acting (e.g., glargine, detemir) or intermediate-acting (e.g., lente) insulins are commonly prescribed for cats.
Dosage & Administration: Initial dosing often starts around 1–2 U per cat, with gradual adjustments based on blood glucose monitoring.
Injection Technique: Shake insulin gently, draw into a U-40 syringe, and inject subcutaneously in the scruff. Rotate injection sites to prevent lipodystrophy.
5. Home Monitoring
Glucose Curve Testing: Owners can capture blood samples at home using glucometers. Repeated readings over 8–12 hours help adjust dosages.
Fructosamine Rechecks: Every 3–4 weeks until stable, then every 3 months to confirm long-term control.
Behavioral & Physical Cues: Monitor for signs of hypoglycemia (tremors, weakness, seizures) or hyperglycemia (persistent thirst, lethargy).
6. Exercise and Weight Control
Encourage Play: Regular interactive play sessions improve insulin sensitivity.
Maintain Healthy Weight: Obese cats are at higher risk for insulin resistance. Structured feeding and controlled exercise help achieve a healthy body condition score (BCS 5/9).
7. Complications & Prognosis
Diabetic Ketoacidosis (DKA): A life-threatening emergency requiring immediate veterinary care.
Neuropathy: Untreated chronic hyperglycemia can cause nerve damage, resulting in hoofed hindlimb paresis (“plantigrade stance”).
Remission Possibility: With stringent dietary control and appropriate insulin therapy, some cats achieve remission—maintaining normal blood glucose without insulin.
Conclusion
Feline diabetes management demands close collaboration between the cat owner and veterinarian. Early detection of symptoms, an appropriate low-carb diet, consistent insulin administration, and diligent home monitoring can help diabetic cats live comfortable, active lives. Always consult your veterinarian for individualized treatment plans.







Comments on "Understanding Feline Diabetes: Symptoms, Diet, and Treatment" :